CMS Promoting RPM by Adding New Codes in 2026
RPM adoption remains limited: Only 30% of U.S. physicians used remote patient monitoring in 2022 (AMA Digital Health Study).
CMS introduced two new RPM codes for 2026, aiming to make RPM more accessible, billable, and clinically valuable for both practitioners and patients.
Why RPM Lagged in Real Practice
1. Reimbursement uncertainty & complex billing: Strict transmission-day minimums, evolving CPT rules, and heavy documentation made adoption difficult.
2. High upfront costs & tech barriers: FDA-cleared devices, HIPAA-secure platforms, and EHR integration were expensive and challenging for small clinics.
3. Workflow burden & staffing constraints: Continuous data review, patient check-ins, and documentation required more staff than many practices could allocate.
New CMS Codes (Effective 2026)
- CPT 99445 (~$47): Covers 2–15 days of short-term RPM data in a 30-day period.
- CPT 99470 (~$26): Covers 10–19 minutes of monthly RPM management time and requires at least one real-time patient interaction.
Impact After Implementation of the New RPM Codes
- Lower entry threshold for small practices.
- Flexible billing aligned with real-world clinical workflows
- Expanded access across primary care, cardiology, endocrinology, nephrology, geriatrics
Real-World Outcomes & ROI Post CMS Code Implementation
-
-
- Patient Panel: 300 CHF, 350 diabetes, 350 hypertension
- Clinical impact:
-
- ~20% reduction in CHF hospitalizations (PMC10424885)
- Improved diabetes & hypertension control (PubMed39974005)
- Increased patient engagement via real-time feedback & monthly interactions
-
- Financial & operational impact (current codes):
-
- Program cost: ~$500/patient/year
- Revenue: ~$700K/year
- Savings from avoided acute events: $400K–$600K
- ROI: ~20–40%, including AI-driven efficiency
-
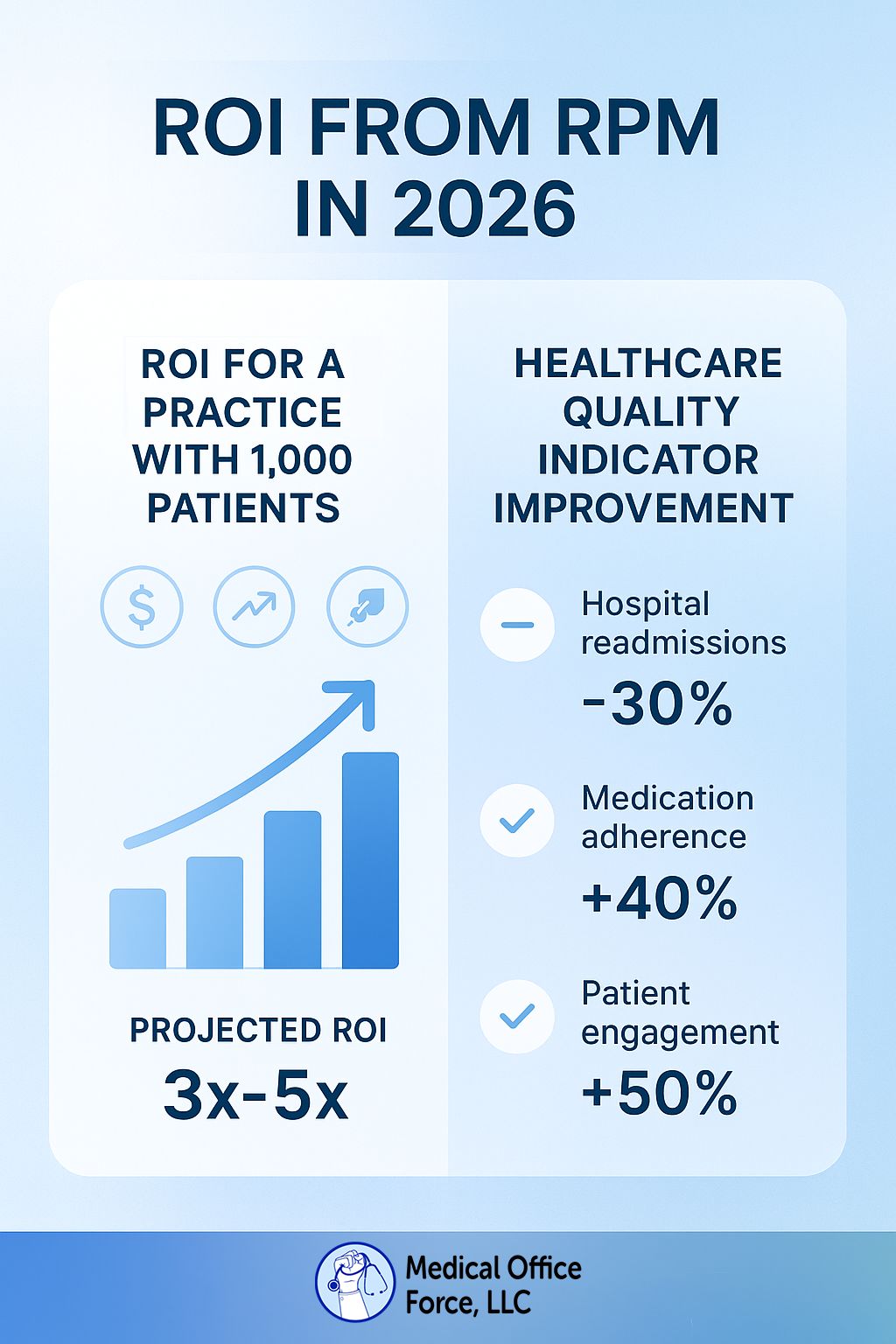
- Projected impact with 2026 codes:
-
- Revenue: ~$900K–$1.1M/year
- ROI: ~300–500%
- Sustained improvements in chronic-disease management.
- Lower hospitalizations, better patient adherence
-
-
Frequently Asked Questions (FAQs)
Q. What is the reimbursement for CPT 99445?
A. The reimbursement for CPT 99445 is approximately $47.
Q. What is the reimbursement for CPT 99470?
A. The reimbursement for CPT 99470 is approximately $26.
Q. When will the new RPM CPT codes take effect?
A. The new Remote Patient Monitoring (RPM) CPT codes take effect on January 1, 2026, as part of the annual 2026 CPT code set updates by CMS.
References:
- CHF RPM study: PMC10424885
- RPM hypertension case: PubMed39974005
- CMS 2026 codes: Federal Register 2025-19787
For more information, write to contact@medicalofficeforce.com


excellent information
These new CMS codes feel like a turning point. Lower thresholds and clearer billing finally make RPM practical for everyday clinical workflows.
Very informative.
Thanks, this was helpful.
Thanks for the insights on the new codes.
This was a very informative read. The breakdown was clear, well-structured, and directly addressed key points. Thank you for sharing valuable insight.
What great information. It’s exciting to see when there are improvements to our services.
It’s refreshing to read a well-balanced discussion on this subject. I’ve also explored these issues recently—feel free to take a look.
Very informative, Thanks for sharing.
Thank you for sharing. It is a great Information.
Very informative and helpful
Thank you for sharing this insightful knowledge!
This is incredibly helpful. Thank you!
Thank you for the valuable information
Very helpful and informative.
“Great breakdown! The new 2026 CMS RPM codes are a game-changer—making adoption easier, boosting ROI, and truly improving patient outcomes.”
Great news , Very informative update. Thanks for sharing.
Truel great and now everyone can be served for the easy access of tech . Now PT can step in with the ease of access.
This is incredibly helpful. Thank you!
Very exhaustive and informative.
INFORMATIVE
This explanation is very clear and informative.
Informative.
Good information it will helpful for us to understand about new upcoming codes it is very informative.
This is very informative.
Thankyou!
Quiet knowledgeable
Great insights! The new 2026 RPM codes truly lower the barriers for practices and make remote care more sustainable. Excited to see how these changes improve patient outcomes and practice ROI.
Helpful breakdown, this makes it clear how the 2026 RPM codes can impact both workflow and patient outcomes.
Great Initiative
Excellent insights — thank you for sharing this information and driving the initiative forward.
Great information! Thank you for sharing this information.
“Very informative update! The 2026 RPM changes will be a game-changer for both providers and patients.”
Thanks for Sharing!!
This is amazing news for all healthcare providers. Thanks for sharing!
Thanks for updating! It is quiet informative!
This blog provides a well-structured and informative overview of CMS’s initiative to expand Remote Patient Monitoring (RPM) through the introduction of new codes in 2026. The explanation of how these codes will support broader adoption, improve care coordination, and enhance reimbursement clarity is particularly insightful. The content is concise, easy to understand, and highlights the practical impact on providers, patients, and healthcare organizations.
Including real-world examples, workflow implications, or estimated financial impacts could make the article even stronger. Overall, this is a valuable and timely update for anyone involved in RPM, telehealth, or revenue cycle management.
There is a great deal to learn about MOF, and thank you for highlighting such important work.
Informative
This is fantastic! The user interface itself appears really tempting, in addition to the contents.
Great Insights. 2026 RPM Updates look very promising.
This is awesome.
Informative.
This is a very essential information update. Thank you for sharing !!!
Thanks for the update, It will very informative & helpful.
Thanks for simplifying the CMS updates. These changes are going to shape the future of digital health.
This is awesome.
The new Remote Patient Monitoring (RPM) program changes, effective January 2026, make it easier for providers to get reimbursed for shorter data collection periods and less clinical time
Awsome
This is great news! This will help more practices that struggle with engagement have more billable patients.
Helpful breakdown, this makes it clear how the 2026 RPM codes can impact both workflow and patient outcomes.
Great information! Thank you!
Very informative, and thank you
Thanks for sharing!
The information is very helpful and gave all the necessary insight of our MOF.
Very Valuable Information. Thanks for sharing!
Thanks for updating. This is beneficial for all!
A much needed change for RPM! Thank you for keeping us informed.
I am glad to hear about the new updates! Thank you for the information!
This is incredibly helpful. Thank you!
This update is a positive step forward—bringing in the new 2026 codes should significantly lower the entry barrier for RPM programs and drive broader adoption across specialties.
Great news! Thank you for the information!
This is highly informative. Thank you for sharing.
Great read, thanks for the information
Thanks for the insights on the new codes.
Very informative and insightful, Thanks for sharing!