Georgia’s $218.8M Rural Healthcare Lifeline: Is Your FQHC Ready?
The safety net is getting a high-tech upgrade. Are you at the table, or on the menu?
Subodh K. Agrawal, MD, FACC
Medical Director, Medical Office Force LLC
As we move into 2026, the story of rural healthcare in Georgia is finally beginning to change. For decades, the narrative has centered on survival, surviving provider shortages, razor-thin margins, and rising patient needs with limited resources. Rural clinics have carried the weight of caring for vulnerable populations while operating in systems that were never designed to support them long term.
Today, however, Georgia stands at a turning point.
With the launch of the GREAT Health Program (Georgia Rural Enhancement and Transformation of Health), the state has been awarded $218.8 million in federal funding. This is not just another funding announcement or pilot initiative. It represents a once-in-a-generation opportunity for Georgia’s Rural Health Clinics (RHCs) and Federally Qualified Health Centers (FQHCs) to modernize how care is delivered, and how sustainability is achieved.
For CEOs and Medical Directors, this moment demands attention. The clinics that prepare and act will shape the future of rural healthcare in Georgia. Those that delay risk falling further behind.
The Real Challenge: Falling Off the Affordability Cliff
Every rural healthcare leader recognizes the pressure building beneath the surface. The expiration of pandemic-era funding and temporary credits, combined with Medicaid unwinding, has pushed uncompensated care to alarming levels. At the same time, workforce shortages have driven labor costs upward, forcing clinics to pay more for fewer available professionals.
Operating on margins of 1 – 2% may have been manageable in the past, but it is no longer realistic under today’s conditions. Clinics are absorbing more risk, delivering more care without reimbursement, and asking already stretched teams to do even more.
This is what many leaders now describe as the “affordability cliff.” Once a clinic reaches it, there is little room for error. Incremental changes are no longer enough. Structural change is required.
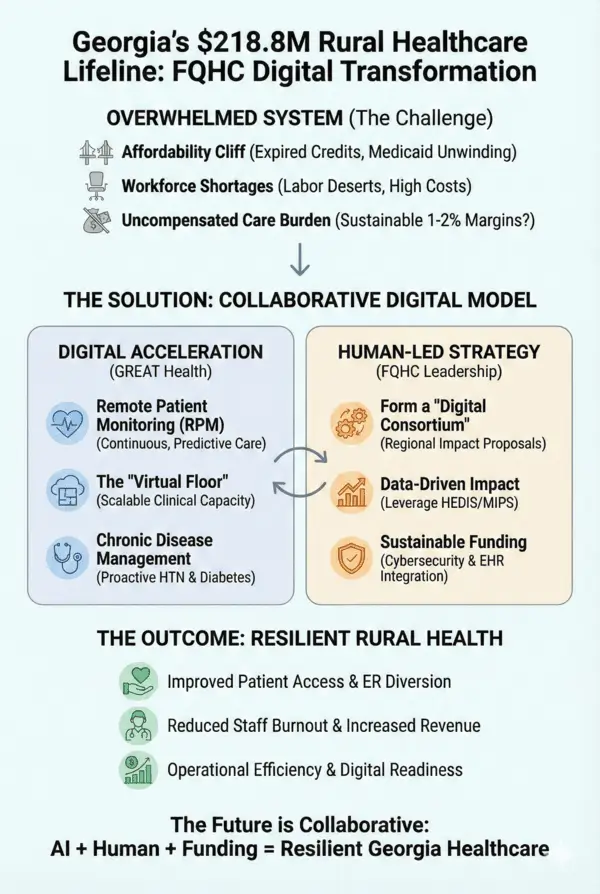
The Opportunity: Digital Acceleration
The GREAT Health funds are specifically earmarked for technology innovation, and that detail matters. Both the Centers for Medicare & Medicaid Services and the Georgia Department of Community Health are signaling a clear priority: rural healthcare must move beyond episodic, visit-based care and toward continuous, data-driven models.
Digital health tools are no longer optional add-ons. They are becoming the foundation of sustainable rural care.
Remote Patient Monitoring (RPM) allows clinics to follow patients between visits, identifying risks early rather than reacting to emergencies. Virtual clinical support, often referred to as a “virtual floor”, helps clinics expand capacity without relying solely on local hiring in already strained labor markets. Chronic disease management programs enable proactive control of hypertension, diabetes, and heart failure, reducing preventable emergency room visits and hospitalizations.
Together, these tools shift care from reactive to predictive, and that shift changes both outcomes and economics.
Why Georgia Received $218.8 Million
A common question among clinic leaders is why Georgia received such a large allocation compared to other states. The answer lies in how the federal government distributes the broader $60 billion Rural Health Transformation fund.
States with large, dispersed rural populations receive greater weight. Georgia also ranks high in Health Professional Shortage Areas (HPSAs) and Medically Underserved Areas (MUAs), indicating deep and persistent access gaps. Historically, Georgia’s non-expansion status contributed to higher levels of uncompensated care, placing additional strain on FQHCs and safety-net providers.
From a federal perspective, Georgia represents both high need and high potential impact. Funding flows where transformation can meaningfully stabilize systems and improve outcomes.
A Consultant’s Playbook: How Clinics Can Maximize Funding
Clinics that succeed in securing GREAT Health funding will not do so by submitting generic applications. They will demonstrate readiness, scalability, and measurable impact.
One effective strategy is forming regional digital consortiums. While individual clinics can apply on their own, collaborative proposals that include multiple RHCs or FQHCs show broader geographic reach and stronger population-level impact. State and federal agencies consistently favor applications that extend benefits beyond a single site.
Equally important is how clinics frame their digital strategy. Funding proposals should move beyond simply requesting devices. Instead, they should clearly articulate how a “virtual floor” will supplement existing teams by providing remote medical assistants, nurses, or care coordinators, roles that are increasingly difficult to fill locally.
Data also plays a critical role. Clinics that leverage existing HEDIS or MIPS data to demonstrate gaps in hypertension or diabetes control, and then commit to specific improvement targets through RPM, align directly with performance-based funding priorities. Increasingly, dollars follow outcomes.
Finally, clinics should not hesitate to request upfront capital for cybersecurity and EHR integration. These are often the biggest barriers to digital adoption, and the Rural Health Transformation framework explicitly allows for such investments.
Why Georgia FQHCs Must Act Now
Timing matters. New 2026 regulations have lowered entry barriers for RPM, including reduced data-day requirements. Revenue that was once bundled into single “catch-all” codes is now unbundled, creating meaningful increases in per-patient monthly reimbursement.
Clinics already using digital care models are seeing measurable reductions in avoidable emergency room visits,often by 20–25%. These reductions protect value-based care incentives while improving patient experience and continuity.
Waiting carries real risk. Patients are increasingly being enrolled in remote programs by large Medicare Advantage plans, sometimes without involvement from their local clinic. When that happens, clinics lose both revenue opportunities and patient relationships.
The Path Forward
We cannot solve the healthcare challenges of 2026 with workflows designed in 1996. Georgia has been given both the resources and the regulatory flexibility to modernize rural care, but funding alone does not create transformation. Leadership does.
The clinics that act now will stabilize their finances, support their workforce, and deliver more consistent, equitable care to the communities that rely on them most. Those that hesitate may find themselves reacting to change rather than shaping it.
FQHC and RHC leaders: What is your biggest barrier to going digital in 2026? Let’s start the conversation.
For more information, write to contact@medicalofficeforce.com


Informative
Quiet Informative!
Very Informative
Very informative and Useful.
Very useful information with great Insights.
Appreciate the update and the clarity provided.
From this blog I got the valid point that we can not solve the healthcare issue or challenges of 2026 with the same pattern or workflows designed in 1996 but Georgia has been given both the resources and the regulatory flexibility to modernize rural care, but funding alone does not create transformation. Leadership does.
Awesome
Very useful information with great analysis
Informative
very enlightening information.
Informative
Clear, informative perspective on Georgia’s rural healthcare opportunity and the importance of digital modernization….,
Looking forward to learning more about the $50 Billion Rural Health Race Plan and the strategy to accelerate growth in rural health
Very informative for the rural health services.
Great initiative, where funding, policy, and technology are finally aligned for rural care.
Great breakdown of Georgia’s $218.8M rural healthcare investment.
This funding highlights that sustainability in rural care now depends on smarter use of technology. Clinics that align digital tools with workforce and reimbursement realities will be far better positioned going into 2026.
Informative.
A rare moment where funding, policy, and technology are finally aligned for rural care.
A timely and compelling perspective. The GREAT Health Program represents a critical turning point for rural healthcare in Georgia, and clinics that act now will be best positioned to drive lasting transformation and sustainability.
True changes with GREAT for RHC’s and FQHC’s.
A great change that really changes the life of RHC’s and FQHC’s and would provide a lot of positive growth.
Great breakdown of Georgia’s Rural Healthcare Lifeline. Important insights for FQHCs navigating funding opportunities in rural communities. Thanks for sharing!
Informative
A truly life-changing experience for rural PT, which really needs to evolve.