
RPM in 2025: What Physicians Need to Know About Getting Paid
As the U.S. healthcare system continues to shift toward value-based care, Remote Patient Monitoring (RPM) is becoming a central piece of the puzzle. In 2025, major changes by the Centers for Medicare & Medicaid Services (CMS) are making it easier and more profitable for providers to get reimbursed for RPM and other care management services.
If you’re a physician, clinic administrator, or billing professional, here’s what you need to know to stay ahead and maximize your revenue.
What’s Changing in 2025?
CMS’s 2025 Medicare Physician Fee Schedule (PFS) final rule has introduced several updates that give RPM and Advanced Primary Care Management (APCM) a major push. The idea is to reward practices that invest in ongoing, personalized care for patients with chronic conditions.
This rule also brings more clarity to coding, billing, and reimbursements, especially for those using virtual care models and serving underserved communities.
Why This Matters: The Push Toward Value-Based Care
Traditional fee-for-service models are slowly being replaced by value-based care. This means providers are now paid for keeping patients healthy and reducing avoidable hospital visits, not just for seeing them in the office.
To support this shift, CMS is encouraging more team-based and continuous care. Remote monitoring and monthly care management are two strategies being heavily promoted.
Understanding APCM: A New Era for Primary Care
Advanced Primary Care Management (APCM) is designed to compensate providers for managing patients in between visits, such as medication tracking, care coordination, and proactive check-ins.
The 2025 final rule introduces new billing levels under APCM:
Level 1: For patients with one chronic condition.
Level 2: For patients with two or more chronic conditions.
Level 3: For patients with multiple chronic conditions and complex needs.
This tiered system lets providers earn more based on the complexity of patient care they deliver.
RPM and APCM
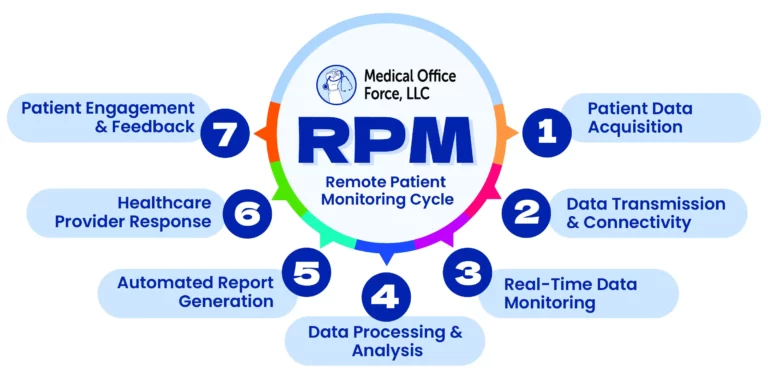
When Remote Patient Monitoring (RPM) is combined with Advanced Primary Care Management (APCM), the real impact is seen in patient health and engagement. By using tools like blood pressure cuffs, glucose monitors, or weight tracking devices, providers can stay connected to patients between visits and respond proactively to any changes in their condition.
This continuous care approach helps identify issues early, prevent hospitalizations, and ensure patients feel supported every step of the way. By layering RPM onto monthly care management, providers can deliver more personalized and timely care, leading to better long-term outcomes, greater patient satisfaction, and a stronger relationship between the patient and care team.
New Billing Codes for 2025
CMS has clarified billing for RPM, CCM (Chronic Care Management), RTM (Remote Therapeutic Monitoring), and BHI (Behavioral Health Integration). In 2025, there will be separate codes for Federally Qualified Health Centers (FQHCs) and Rural Health Clinics (RHCs), making it easier for providers in underserved areas to get paid.
Key RPM CPT Codes to know:
99453 – Initial setup and patient education
99454 – Device supply and data transmission (30 days)
99457 – 20 minutes of care team time (interactive communication)
99458 – Each additional 20 minutes
These codes support billing for both virtual and in-person care.
Good News for FQHCs and RHCs
1. Supports monthly billing of RPM and RTM
2. Encourages clinics to invest in virtual care technology
3. Offers a higher payment rate under value-based models
4. Helps reduce care gaps in rural and underserved communities
It’s a huge win for providers who were doing this work without getting fully paid.Virtual Care Is Here to Stay
The COVID-19 pandemic fast-tracked telehealth adoption. Now, CMS is making some of those temporary policies permanent. Virtual check-ins, RPM, and monthly remote care management are no longer just nice-to-have—they’re essential services.
In 2025, CMS clarified:
1. Virtual care is reimbursable with proper documentation
2. RPM must be used for at least 16 days per month to qualify
3. All care plans must be ordered by a qualified professional
4. Patient engagement and shared decision-making are strongly encouraged
If your practice isn’t using RPM yet, now is the time to start.
Key Takeaways for 2025
Here’s what your practice should focus on this year:
Adopt RPM tools like blood pressure cuffs, glucose monitors, or wearables
> Train your care team to manage care between visits
> Document properly using the new CPT and HCPCS codes
> Serve underserved populations with G0511 billing (for FQHCs/RHCs)
>Combine RPM with APCM for maximum reimbursement
>Use care coordinators and technology to streamline workflows
Final Thoughts: Get Ready Now
As CMS rolls out transformative changes in 2025, it’s more important than ever for healthcare providers to align with the new reimbursement models and optimize care delivery. Medical Office Force (MOF) is at the forefront of this transition, helping practices integrate Remote Patient Monitoring (RPM), adopt Advanced Primary Care Management (APCM), and capitalize on new billing opportunities. By offering a combination of expert RCM services, trained virtual staff, and workflow optimization strategies, MOF ensures that providers not only comply with the new regulations but also thrive in a value-based care environment.
Want help implementing RPM or optimizing your billing workflows? Medical Office Force is here to support you with expert RCM services, denial management, and virtual staffing solutions. Let us help you get paid—accurately and on time.
- Posted on - April 21, 2025


For more information, write to contact@medicalofficeforce.com
Share Your Thoughts
No comments yet — be the first to comment!