
The $100M Pivot: Why Centers for Medicare & Medicaid Services Just Supercharged Chronic Care Management
Subodh K. Agrawal MD,FACC
Medical Director, Medical Office Force LLC
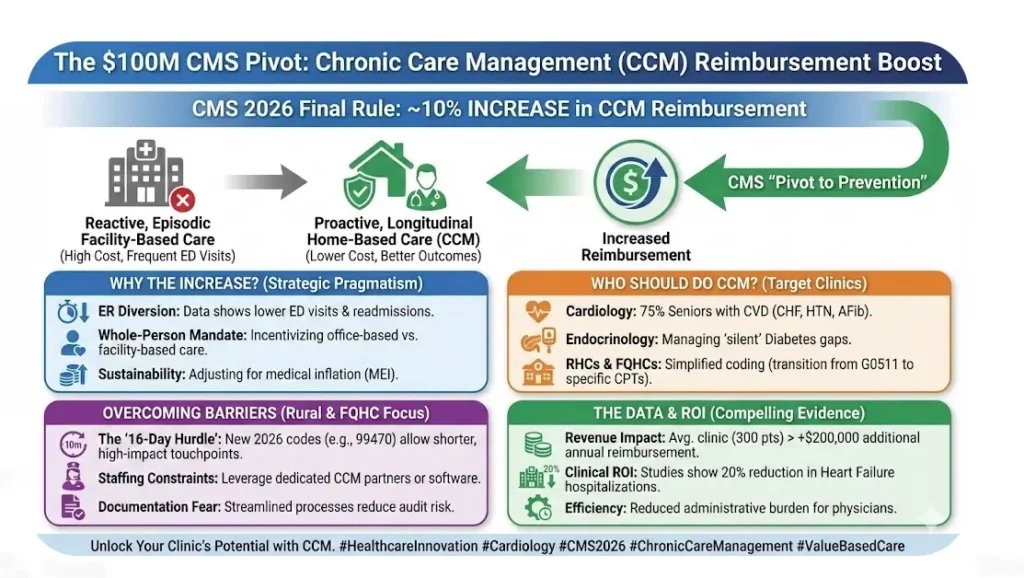
For months, healthcare leaders prepared for tightening Medicare margins. Instead, the 2026 Final Rule introduced a strategic shift that many practices have underestimated. The Centers for Medicare & Medicaid Services increased reimbursement for Chronic Care Management by nearly 10 percent. This is more than a rate adjustment. It is a clear signal about how care delivery will be valued moving forward.
For years, CCM has existed in the background. Many clinics viewed it as optional or administratively heavy. In reality, it has now become one of the most stable and predictable revenue streams available to practices managing complex Medicare populations.
Why CMS Made This Move
The logic is economic and clinical. Proactive care costs less than reactive care.
Patients enrolled in structured Chronic Care Management programs consistently demonstrate lower emergency department utilization and fewer hospital readmissions. When chronic conditions such as heart failure, diabetes, hypertension, or atrial fibrillation are monitored between visits, complications are addressed earlier. Medication adherence improves. Small issues are managed before they escalate into hospital level events.
CMS is not simply increasing payment. It is redirecting the healthcare system away from episodic, facility centered care and toward continuous, office based longitudinal management.
Another driver is sustainability. Medical Economic Index growth continues to pressure practice expenses. Staffing costs, technology investments, compliance demands, and reporting obligations have all increased. Visit based reimbursement alone cannot sustain complex panels of elderly patients with multiple comorbidities. By strengthening CCM rates, CMS is acknowledging the real work required between face to face visits.
Cardiology: The Strategic Advantage
While primary care traditionally leads CCM adoption, cardiology is uniquely positioned to benefit under the new framework.
Nearly three quarters of seniors live with some form of cardiovascular disease. Conditions such as congestive heart failure, coronary artery disease, hypertension, and atrial fibrillation require constant oversight. Medication titration, symptom tracking, lifestyle reinforcement, and coordination with primary care are ongoing processes.
Cardiologists already manage this complexity. CCM simply formalizes and reimburses the time spent doing it.
Instead of uncompensated follow up calls, medication checks, and coordination efforts, practices can structure monthly care management protocols that improve patient engagement and generate predictable recurring revenue. In a specialty heavily impacted by Medicare reimbursement shifts, CCM can act as a stabilizing financial pillar.
The Rural and FQHC Opportunity
Rural Health Clinics and Federally Qualified Health Centers stand at an important inflection point. Historically, many relied on broad bundled codes that did not fully reflect the intensity of chronic care management work. The transition away from older structures toward specific CPT based billing creates clarity and stronger reimbursement alignment.
Yet adoption in rural settings has lagged.
Why? Operational friction.
Tracking required time thresholds was viewed as cumbersome. Many clinics lacked a dedicated nurse to handle monthly outreach. Documentation requirements felt intimidating, particularly for lean teams concerned about audit exposure.
The 2026 updates ease some of these barriers. Shorter high impact touchpoints can now qualify under revised structures, reducing the rigidity of previous thresholds. When supported by structured workflows or dedicated CCM software platforms, documentation becomes standardized rather than overwhelming.
For rural clinics operating on thin margins, CCM may represent one of the few scalable revenue enhancements that does not require additional physical infrastructure.
Addressing Common Hesitations
Many physicians remain skeptical. The concerns are familiar.
“We do not have staff.”
“We do not want audit risk.”
“We are already overwhelmed.”
These concerns are valid. However, they reflect workflow design challenges rather than program flaws.
CCM does not require physicians to personally complete every minute of monthly engagement. Clinical staff operating under supervision can perform structured outreach, medication reconciliation, and care plan updates. Documentation templates reduce variability and audit risk. External CCM partners can support outreach if internal staffing is constrained.
The key is operational discipline.
The Financial Case
Consider a mid-sized cardiology clinic with 300 eligible Medicare patients enrolled in CCM. Under updated reimbursement rates, incremental annual revenue can exceed $200,000. This is recurring, predictable income tied directly to patient engagement rather than procedural volume.
In a climate where procedure reimbursement faces volatility, this diversification matters.
But revenue alone should not drive the decision.
The Clinical Return on Investment
Studies consistently demonstrate that structured chronic care management reduces hospitalizations among heart failure populations. When patients receive regular check ins, medication reviews, and early intervention, adverse events decline.
Improved outcomes translate into stronger quality metrics, better patient satisfaction, and alignment with value based payment models. As Medicare continues to emphasize risk adjustment and population health accountability, CCM becomes strategically aligned with broader system direction.
This is not a temporary incentive. It is part of a long term payment transformation.
The Bottom Line
Chronic Care Management is no longer a side program. It is a cornerstone of modern outpatient practice.
The 2026 Final Rule makes one thing clear: CMS intends to fund proactive, coordinated care. Practices that build structured CCM programs will stabilize revenue, strengthen patient relationships, and reduce avoidable acute events.
Those that ignore it will continue absorbing uncompensated care coordination while margins compress.
The pivot has already occurred. The only remaining question is whether your organization is positioned to capitalize on it.
For more information, write to contact@medicalofficeforce.com


The CCM program is highly beneficial for patients and strengthens the relationship with the providers for managing healthcare. Thank you for sharing the blog.
I am glad that this article highlights the benefits of the CCM program since it is a wonderful program that should be a part of every practice.
Great news!
Informative
Great information