RPM Is Not a Device Program, It Is a Care Model
Remote Patient Monitoring, or RPM, is often misunderstood. Many people believe RPM simply means giving patients a device, such as a blood pressure monitor or glucose meter, and collecting readings. In reality, RPM goes far beyond devices and data. When implemented correctly, it is a care model that improves outcomes, strengthens patient relationships, and helps providers deliver continuous care beyond the clinic.
At Medical Office Force, we believe RPM works best when it is treated as a care first approach rather than a technology driven program.
What Is RPM
RPM allows healthcare providers to track patient health data outside traditional office visits. This includes blood pressure, blood glucose, weight, oxygen levels, and heart rate. Patients use FDA approved devices at home, and data is securely shared with the care team. This enables providers to monitor trends, identify risks early, and intervene before conditions worsen. RPM is not just about collecting numbers, it is about acting on them.
Why RPM Is Often Treated Like a Device Program
Many RPM programs underperform because the focus stays on shipping devices, meeting compliance requirements, billing CPT codes, and collecting data without patient engagement. When RPM becomes a set it and forget it program, patients stop using devices, data goes unread, and outcomes do not improve. This is not a failure of technology, but a failure of care delivery.

RPM as a Care Model
A true care model focuses on people, processes, and outcomes, not just tools. When RPM is implemented correctly, it includes patient education, regular communication, clinical review of data, care coordination, timely interventions, and proper documentation. RPM becomes an extension of the clinical team rather than a separate technology initiative.
Care Beyond the Office Visit
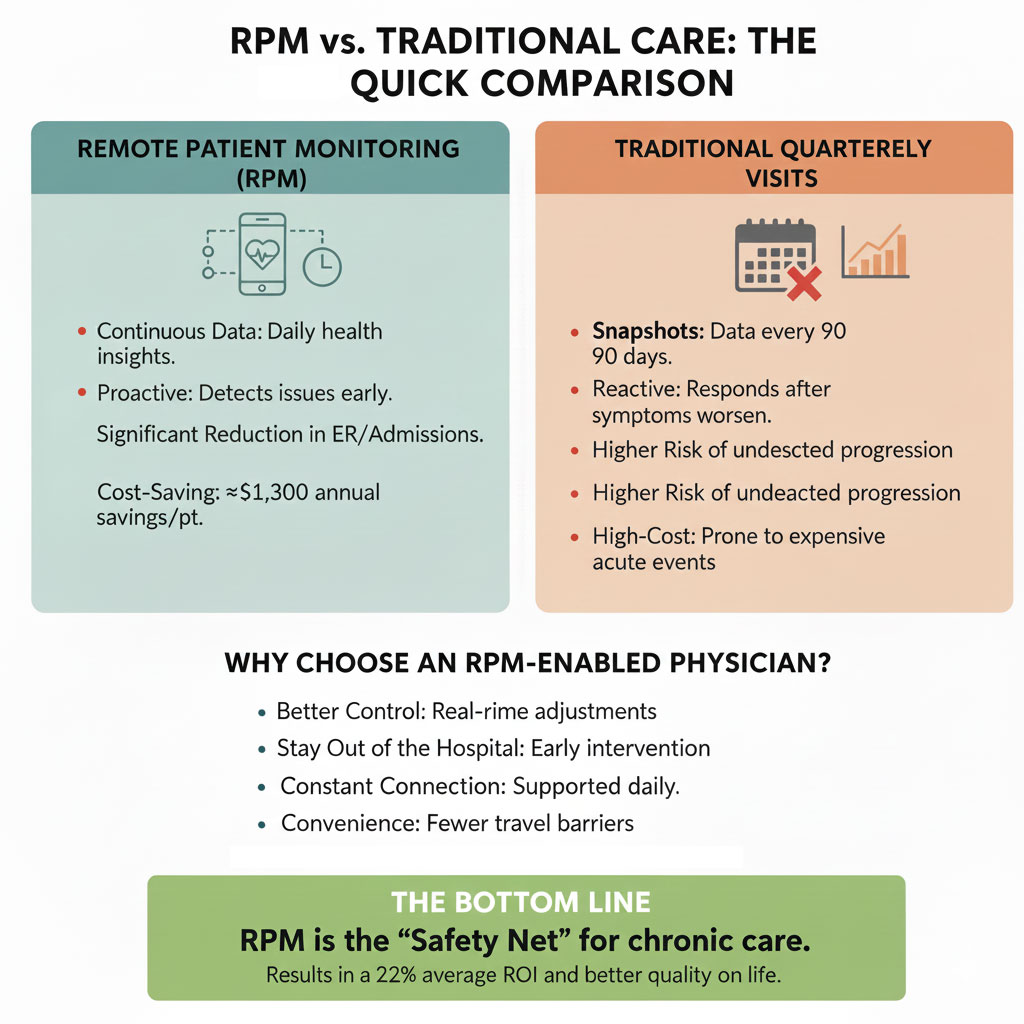
Traditional care is visit based. Providers often have limited visibility into a patient’s condition between appointments. RPM changes this by enabling continuous care. Providers see trends rather than single readings, patients feel supported between visits, and potential problems are identified early. This shift from visit based care to continuous care is where RPM delivers real value.
Patient Engagement and Clinical Oversight
Devices do not engage patients, people do. A successful RPM program ensures patients understand why monitoring matters, know how to use their devices, and receive regular feedback. When patients know their data is reviewed and their progress matters, adherence improves naturally.
Clinical oversight makes RPM meaningful. Trained staff review readings, follow up on abnormal values, and provide providers with clear, actionable insights. This ensures RPM supports decision making rather than overwhelming care teams with raw data.

Supporting Chronic Care and Coordination
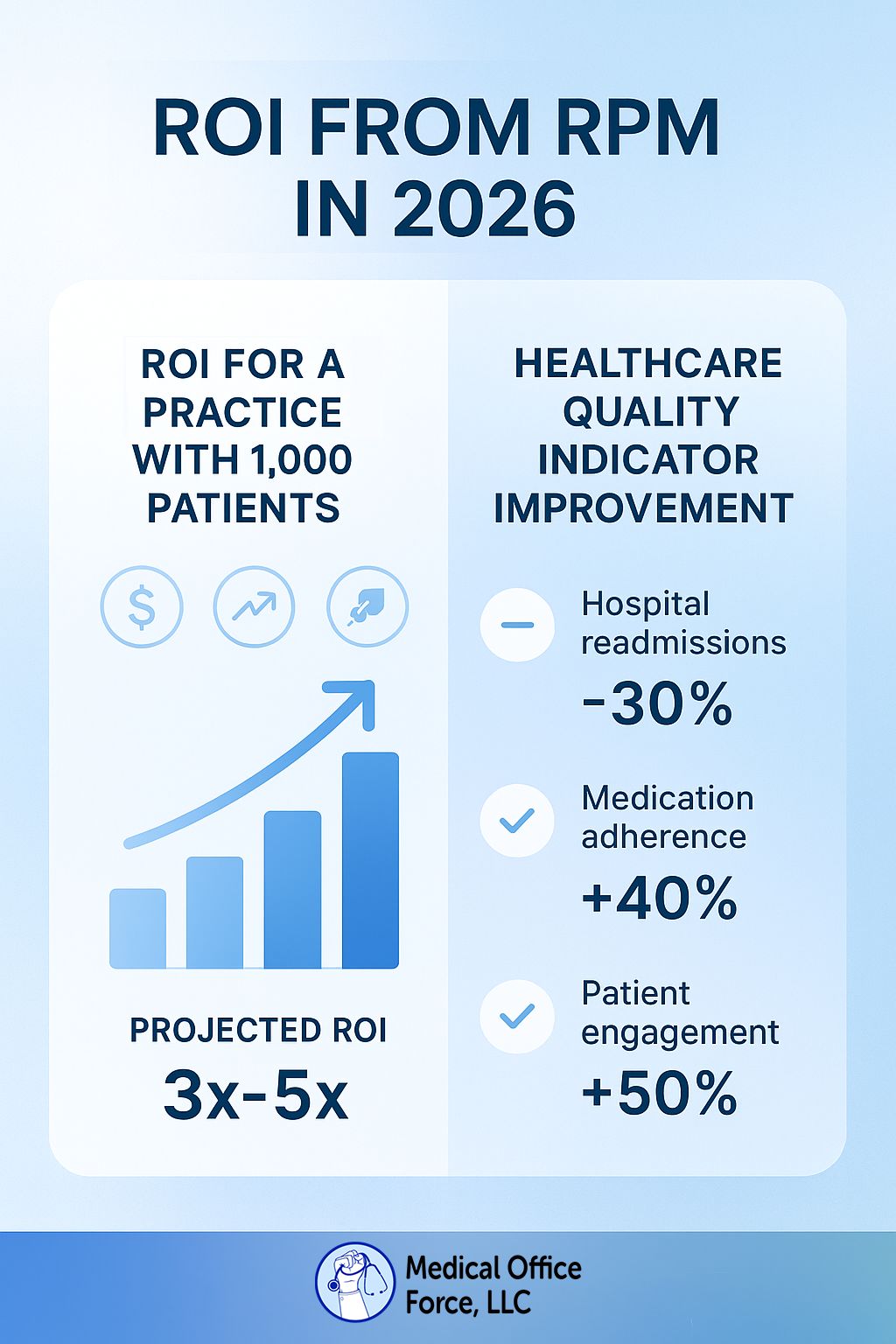
RPM is especially effective for chronic conditions such as hypertension, diabetes, heart disease, COPD, and obesity. These conditions require consistent monitoring and long term support. RPM helps providers track progress between visits, adjust care plans proactively, improve medication adherence, and build stronger patient relationships.
When RPM integrates smoothly into existing workflows, including clear escalation protocols and accurate documentation, it strengthens the entire practice and aligns well with value based care initiatives.
Technology Supports Care, Not the Other Way Around
Technology plays an important role in RPM, but it does not replace care. Like a stethoscope, devices are only valuable when paired with clinical expertise, thoughtful workflows, and consistent follow up. RPM succeeds when technology supports human care.
Final Thoughts
RPM is not a device program, a data collection tool, or a billing strategy. It is a care model. When implemented with the right mindset and support, RPM helps patients feel connected, providers stay informed, and care extends beyond the clinic walls.
At Medical Office Force, we help practices build RPM programs that prioritize care, engagement, and outcomes, because technology works best when it supports human care.