7 Things to Check Before Starting CCM, RPM, or RTM
If you’re a doctor or clinic owner looking to improve patient care and grow your revenue, programs like Chronic Care Management (CCM), Remote Patient Monitoring (RPM), and Remote Therapeutic Monitoring (RTM) are great opportunities. But before you jump in, there are a few things you should check to make sure you’re set up for success.
In this blog, we’ll explain 7 simple things you should check before starting any of these programs.
1. Do Your Patients Qualify?
Before anything else, you need to know which patients are eligible:
- CCM: Patients must have 2 or more chronic conditions like diabetes, hypertension, or COPD.
- RPM: Patients must need regular health monitoring using a device.
- RTM: Great for patients with muscle, joint, or lung issues who need help following therapy plans using apps.
Why this matters: If a patient doesn’t qualify, Medicare or insurance may not pay you.
Look through your EHR and flag eligible patients. Most clinics already have dozens of patients who qualify but haven’t been enrolled yet.
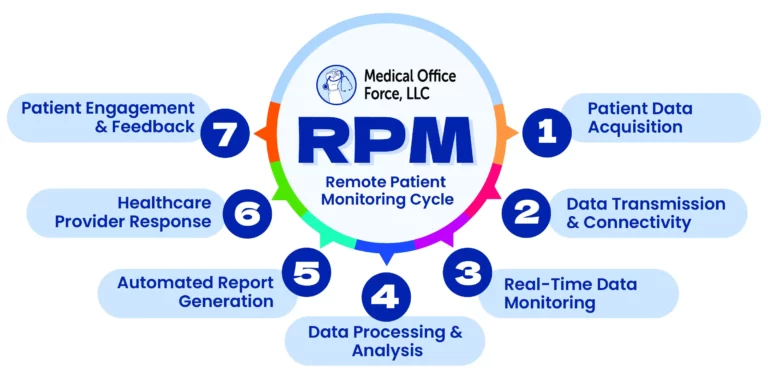
2. Pick the Right Technology
The success of CCM, RPM, and RTM depends heavily on good technology. You need tools that:
- They are easy for patients to use
- Track and record time spent with patients
- Send alerts when something needs attention
- Are HIPAA compliant and secure
For RPM, make sure the device works automatically
For RTM, make sure the app helps patients report how they’re feeling and if they’re following therapy.
Ask for a demo before you commit. A confusing system = frustrated staff and patients.

3. Train Your Team
Even with the best tech, your program won’t work if your team isn’t ready. Make sure to:
- Train nurses and staff on what each program is
- Show them how to track time, check data, and follow up
- Explain what to do when a reading is too high or too low
Assign a CCM/RPM coordinator who can manage communication with patients and track monthly time.
4. Understand How You Get Paid
These programs pay you based on time and service. Here’s a rough idea:
- CCM: Around $62 to $125/month per patient
- RPM: Around $ to $200/month per patient
- RTM: Around $ to $180/month per patient
But you must:
- Track time correctly (minimum of 20 minutes for CCM and 16 days of data for RPM)
- Use the correct CPT billing codes
- Get patient consent (usually verbal or written)
- Compliant report generation monthly
Talk to your billing team or partner with a company that specializes in these services to avoid mistakes.
5. Help Patients Understand and Join
Many patients won’t know what CCM, RPM, or RTM means. Make it simple:
1. Explain that it’s a monthly check-in or health support service
2. Show them the device or app they’ll use
3. Let them know it helps keep them out of the hospital
Have a friendly team member walk them through it. Give them a printout or video that explains what they’re signing up for.
Medical Office Force will help with onsite registration and patient education to keep your staff focused on your practice.
For older patients, offer to help them set up the device or app during a visit.
6. Keep Good Records
If you’re billing Medicare, you need to keep records of:
1. Patient consent
2.Time spent on care coordination or reviewing data
3. Any actions you take (calls, alerts, medication reviews)
If you don’t have proof, you could fail an audit and have to return payments.
Use software that automatically tracks everything. It saves time and keeps you safe.

7. Decide: Do It Yourself or Get Help?
Running these programs in-house takes time, people, and tools. If you’re already busy, consider outsourcing to experts.
You can:
1. Do everything in-house
2. Get help from a CCM/RPM service provider (like Medical Office Force)
3. Start small and grow over time
Outsourcing can help you launch faster with fewer headaches, especially at the start.
Final Thoughts
CCM, RPM, and RTM can truly change the way your practice works:
1. Better patient care
2. Fewer hospital visits
3. More monthly revenue
But success depends on proper planning.
1. Check patient eligibility
2. Choose smart tools
3. Train your team
4. Understand billing
5. Help patients onboard
6. Track everything
7. Know when to outsource
Need help getting started? Medical Office Force offers full support to help you launch, manage, and grow your remote care programs. Let’s work together to make it easy and profitable!
Visit www.medicalofficeforce.com to learn more.